The Quality Standards Resource Centre helps extend understanding of the strengthened Aged Care Quality Standards, which took effect from 1 November 2025. You can search for resources by using keywords, or filtering by standard, outcome and audience. Before using the Resource Centre, please read the terms of use.
Recognising Signs of Deterioration in a Person’s Mental State
This resource provides a framework for recognising signs of mental state deterioration, organised into 5 key indicators: reported change, distress, loss of reality, loss of function, and elevated risk. It supports healthcare providers in monitoring mental health changes to enable timely and effective responses across care settings. This resource may apply to healthcare contexts outside of aged care. Please consider the applicability of this resource to your care setting.
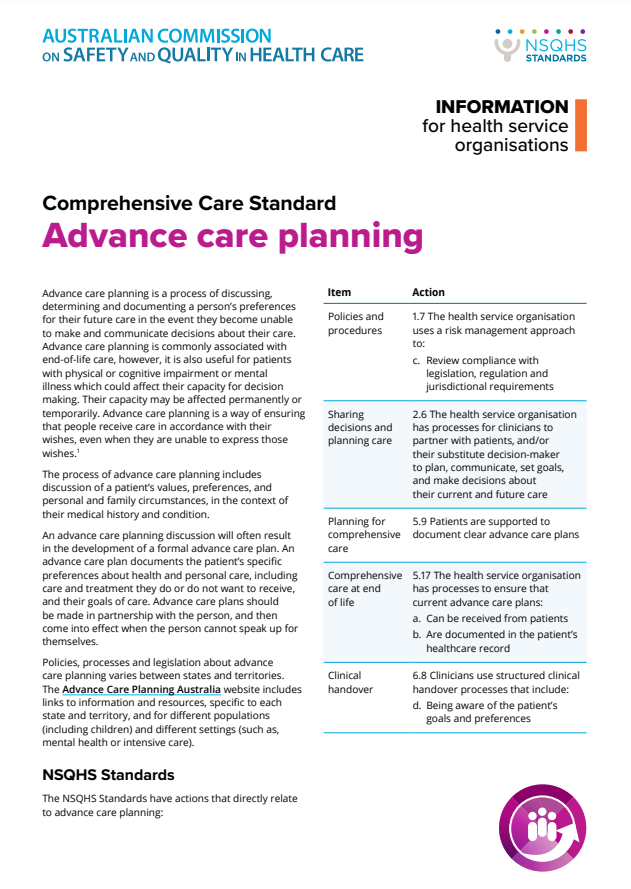
Advance care planning - Information for health service organisations
This resource outlines how health service organisations can support advance care planning within the Comprehensive Care Standard (National Safety and Quality Health Service Standards). It highlights the importance of documenting a patient’s preferences for future care and ensuring systems are in place to act on these plans. It also provides actions related to policies, sharing decisions, comprehensive care, and clinical handover.
Informed consent
This resource provides guidance on ensuring informed consent in healthcare settings. It outlines legal, ethical, and professional requirements for obtaining consent, supports person-centred care, and ensures compliance with Australian healthcare standards. It highlights the importance of providing accurate information about interventions and alternatives, ensuring people have sufficient knowledge of potential risks and benefits.
Advance care planning - Information for clinicians
This resource guides clinicians on the importance of advance care planning, particularly for those with life-limiting illnesses, chronic conditions, or cognitive impairment. It outlines the need for early conversations about patient preferences and comprehensive care, ensuring decisions are documented, shared, and align with clinical handover processes to respect patient autonomy and improve care outcomes.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Comprehensive Care - Clinical assessment and diagnosis - Key actions for health service organisations
This resource provides actions for health service organisations to support clinical assessment and diagnosis, promoting a person-centred approach and comprehensive care planning. It highlights training, clear communication of roles, and systems for documenting diagnoses and care plans.
This resource may apply to healthcare contexts outside of aged care. Please consider the applicability of this resource to your care setting. This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Comprehensive Care - Clinical assessment and diagnosis - Key actions for clinicians
This resource provides actions for health service organisations to support clinical assessment and diagnosis, promoting a person-centred approach and comprehensive care planning. It highlights training, clear communication of roles, and systems for documenting diagnoses and care plans.
This resource may apply to healthcare contexts outside of aged care. Please consider the applicability of this resource to your care setting. This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
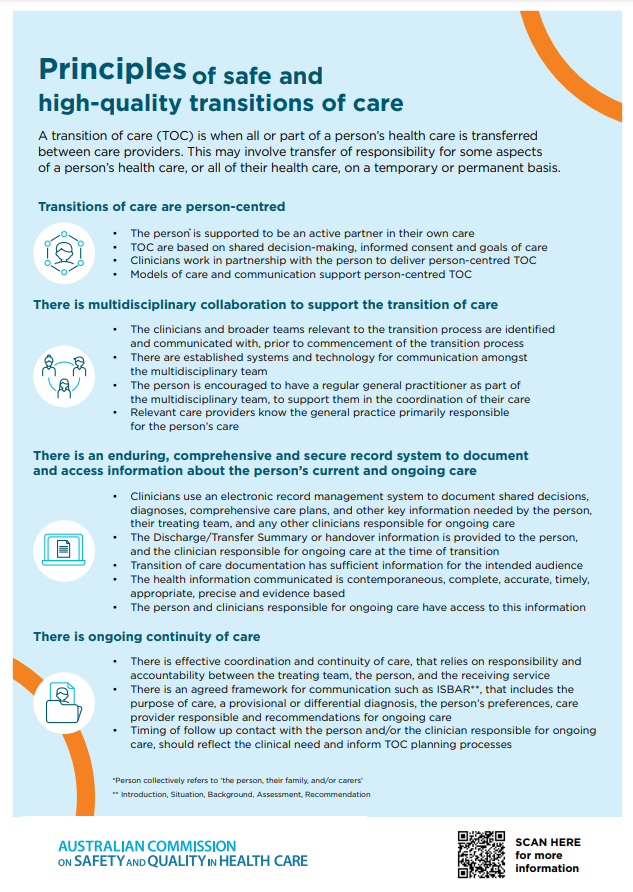
Fact sheet - Principles of safe and high-quality transitions of care
This resource outlines the principles for safe and high-quality transitions of care, emphasising person-centred care, multidisciplinary collaboration, and effective communication. It highlights the need for secure documentation, continuity of care, and coordination among healthcare teams to make sure smooth transitions and minimise risks during transfers between care providers.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Essential element 2: Identifying goals of care
This resource guides providers in identifying and setting goals of care with patients through shared decision-making. It fosters collaboration between patients, family, and healthcare teams to clarify expectations and establish personalised clinical and personal care objectives.
This resource may apply to healthcare contexts outside of aged care. Please consider the applicability of this resource to your care setting. This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Comprehensive Care - Review and improve comprehensive care delivery - Key actions for health service organisations
This resource outlines actions for health service organisations to review and improve comprehensive care delivery, focusing on aligning care with patients' needs and care plans. It emphasises regular assessment, multidisciplinary collaboration, and quality improvement to maintain responsive, person-centred care across services.
Communication at clinical handover
This resource focuses on structured clinical handover processes to improve communication during patient care transitions. It highlights the importance of standardising handover procedures to make sure relevant information is effectively communicated, reducing errors and enhancing patient safety, especially during care transfers in healthcare settings, including aged care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.

Cognitive impairment resources
This resource provides a range of materials developed to improve the safety and quality of healthcare for people with cognitive impairment or at risk of delirium. It includes guides, fact sheets, and standards for consumers, clinicians, and health service organisations, supporting the implementation of best practice and quality care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Communicating for Safety
This resource provides tools and guidance on improving clinical communication to enhance patient safety. It focuses on key communication touchpoints, such as handovers, decision-making, and care transitions. Designed to support healthcare providers, it offers practical strategies to reduce errors and improve outcomes in aged care and other healthcare settings.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Principles for safe and high-quality transitions of care
This resource outlines essential principles to support safe and high-quality transitions of care for people across healthcare settings, including aged care. It emphasises person-centred approaches, multidisciplinary collaboration, secure record systems, and continuity of care, aiming to minimise risks during care transitions for vulnerable populations.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Poster - Principles of safe and high-quality transitions of care
This resource outlines the principles of safe and high-quality transitions of care. It highlights the importance of person-centred care, multidisciplinary collaboration, and clear communication between providers. It ensures coordination, accountability, and secure documentation to support continuity of care when transferring people between care settings. This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.

National Consensus Statement - Essential elements for recognising and responding to acute physical deterioration
This consensus statement outlines essential elements for recognising and responding to acute physiological deterioration in healthcare settings. It covers clinical processes like vital signs monitoring, diagnosis, and rapid response systems, as well as organisational aspects such as leadership, education, and evaluation. It provides generic information that can be applied to the aged care setting.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Case study - Safe and Appropriate use of Psychotropic Medicines - Residential Aged Care
This resource is a fictional scenario that follows an older person’s care pathway with a residential aged care provider. The resource focuses on the systems and processes to support high-quality care of older people living with cognitive impairment. It includes 4 key priority areas: person-centred care, medication management, managing changed behaviours and transitions of care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Case study - Safe and Appropriate use of Psychotropic Medicines - In-home Aged Care
This resource is a fictional scenario that follows an older person’s care pathway with an in-home aged care provider. The resource focuses on the systems and processes to support high-quality care of older people living with dementia. It includes 4 key priority areas: person-centred care, medication management, managing changed behaviours and transitions of care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Safe and appropriate use of psychotropic medicines for aged care - Fact sheet
This fact sheet is informed by the Psychotropic Medicines in Cognitive Disability or Impairment Clinical Care Standard (CCS), developed by the Australian Commission on Safety and Quality in Health Care. The CCS describes the safe and appropriate use of psychotropic medicines for people with cognitive disability or impairment, in a way that upholds their rights, dignity, health and quality of life.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
NSQHS Standards User guide for Aboriginal and Torres Strait Islander health
The resource provides a guide for health service organisations to improve care for Aboriginal and Torres Strait Islander people, focusing on 6 specific actions. It highlights strategies to build partnerships, enhance cultural competency, and ensure equitable, safe, and high-quality care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.
Implementing the Comprehensive Care Standard - Clinical assessment and diagnosis
This document provides guidance on implementing the clinical assessment and diagnosis element of the Comprehensive Care Standard (National Safety and Quality Health Service Standards). It helps clinicians identify a person’s conditions or needs through examination and investigation. The resource supports safe, patient-centred care, improving diagnostic accuracy and promoting teamwork in healthcare settings, including aged care.
This resource may refer to information that will be updated from 1 November 2025 to align with the new Aged Care Act and Quality Standards.