Commissioner’s message
Vaccinations
While the pandemic continues, the high levels of COVID vaccination among those receiving aged care and those working in aged care services around the country are helping to reduce the risk of serious consequences from the virus for both consumers and staff.
As recently announced, the expert Australian Technical Advisory Group on Immunisation (ATAGI) is now recommending an additional COVID-19 vaccine dose for residents in aged care services before winter. This is a second booster dose, bringing the total number of recommended doses to 4. ATAGI recommends that residents receive their COVID-19 winter dose from 4 months after their initial booster dose. This fourth dose is intended to bolster residents’ protection from severe illness, hospitalisation or death from COVID-19 over the winter season.
Residential aged care providers are required to make arrangements now for COVID-19 winter dose vaccinations for your residents and eligible workers. The options available to providers for accessing this winter dose are set out in advice published by the Department of Health.
It is important to note ATAGI’s advice that COVID-19 winter doses can be administered at the same time as the annual flu vaccination. Administration in the same session of separate COVID-19 winter doses and influenza vaccines for residents is both clinically safe and administratively efficient. Consequently, in planning your winter vaccine program, residential aged care providers are encouraged to:
- identify and optimise opportunities for concurrent administration of COVID-19 winter doses and flu vaccines where possible
- not delay the administering of flu vaccines to residents if concurrent administration is not possible or is likely to delay flu vaccination.
Visitor access
Another pandemic-related issue that requires attention relates to visitor access. Some aged care providers are still placing significant limitations on family members’ access to residents – well beyond any directions contained in a public health order.
Residential care settings are the homes of residents, who should be supported to maintain relationships and engage in social contact. Experiences of lockdowns in a number of aged care homes over the last 2 years have underscored the potentially damaging physical, psychosocial and nutritional impact on older people of extended periods of social isolation. In line with advice provided by the Australian Health Protection Principal Committee (incorporated in the Industry Code for Visiting in Aged Care Homes, updated in March 2022), residential aged care providers must facilitate access to their premises by people who are part of residents’ lives and who matter to them. The Commission’s fact sheet, Ensuring safe visitor access to residential aged care, provides further guidance on this important issue.
Governing for Reform in Aged Care program open
The Commission-led Governing for Reform in Aged Care learning program was launched on 16 March by Minister for Senior Australians and Aged Care Services, Senator the Hon Richard Colbeck. The Minister was joined by the Commissioner Janet Anderson, and sector leaders Mike Baird, Chief Executive Officer HammondCare, Anne Skipper, Chair Silver Chain and Maree McCabe, Chief Executive Officer Dementia Australia.
The 3-member panel of sector leaders discussed the changes needed in the aged care sector, the importance of leadership and good governance in delivering change, and how the learning program can help members of governing bodies and executives navigate the reform agenda and enhance consumer outcomes in their organisations.
The program launch webinar recording is available for those who could not attend the session or who would like to revisit the discussion.
The Commission is encouraging all aged care providers to play your part in this once-in-a-generation opportunity to reform the aged care sector and enhance consumer outcomes by enrolling in the free learning program today.
Participants can access information about the program, how it will be delivered and, once enrolled, complete the diagnostic tool and share program information with their board and network.
Commission’s upcoming roundtable discussions
Enriching the lives of older Australians through aged care is a worthy aspiration for everyone working in the aged care sector. Alongside the formal learning program outlined in the previous article, the Commission will soon be inviting board chairs and chief executive officers of aged care providers to join us in a series of roundtable discussions to consider what decisions and actions are available to providers that would move them closer to achieving this vision.
The roundtable program will offer providers across the country the opportunity to connect online or face-to-face with our Commissioner Janet Anderson and Assistant Commissioner Lisa Peterson to discuss:
- engaging with consumers to understand their expectations and wishes for their aged care experience
- enabling a positive workplace culture that shapes the aged care experience to be best practice
- measuring performance and benchmarking relative to other providers and to the expectations of your care recipients
- planning and driving the continuous improvement of aged care services.
We will also welcome attendees’ ideas on how the Commission can better frame and target information, education and networking resources to support sector capability uplift.
If you’re a board chair or Chief Executive Officer, we will soon send you an invitation about these roundtable discussions and let you know how you can register your interest to attend.
Incident management system essential element #2 – Responding to incidents
The February Quality Bulletin included our first article about the essential elements of an effective incident management system (IMS), focusing on ensuring leadership and a safety culture.
In this next article in our series, we look at the second element that residential aged care and home care providers must have in their IMS.
IMS essential element #2 – Responding to incidents
You have 2 primary tasks when responding to incidents or near misses at your service – you need to identify the incident and immediately support anyone affected by it.
You may identify an incident or near miss in several ways, including when:
- a staff member or another consumer observes it
- a consumer discloses it
- someone else tells a staff member about it.
Be aware that some incidents may be harder to identify or confirm, especially if they involve abuse, neglect or they’re disclosed by a consumer with cognitive impairment. A suspicion or allegation of an incident is just as important to respond to as a witnessed incident.
Near misses may also be hard to identify – but they are nonetheless important to note and report. A near miss is when an occurrence, event or omission happens that does not result in harm (such as injury, illness or danger to health) to a consumer or another person, but it had potential to do so. Near misses provide an important learning opportunity in relation to what must be done differently to reduce the risk of such an incident.
As an aged care provider, you have a responsibility to:
- ensure your staff are trained and equipped to identify and report incidents and near misses when they occur
- take all incident disclosures seriously (including suspicions and allegations) and investigate them appropriately to determine whether an incident occurred.
When an incident has occurred, you must take immediate action to assess the support required by those affected.
As part of this assessment, you should consider the level of harm or impact on anyone involved in the incident, and what actions are needed to reduce this harm and ensure their health, safety and wellbeing.
It is good practice for you to have a response plan for dealing with incidents when they occur. The response plan could include that, as the provider, you will:
- act immediately with people involved in the incident – for example, provide them with physical or psychological treatment or support
- engage with people affected by the incident to determine an appropriate response – for example, notify a consumer’s representatives or coordinate access to advocates
- assess and ease any risks to others that could be affected by the incident – for example, support any witnesses
- decide what to do if the incident is (or may be) a reportable incident – for example, notify the Commission or the police.
More information
Read our ‘Effective incident management systems: Best practice guidance’ for information about how you can develop and embed an IMS in your service.
Joint action to reduce the inappropriate use of psychotropic medicines
The Commission has partnered with the NDIS Quality and Safeguards Commission and the Australian Commission on Safety and Quality in Health Care to release a joint statement committing to collective action to address and reduce the misuse and overuse use of psychotropic medicines in the aged care and disability sectors.
The statement provides a framework for future work and collaboration across the sectors and outlines the roles of the 3 Commissions in undertaking further actions. The Royal Commission into Aged Care Quality and Safety identified an over-reliance on chemical restraint as a priority concern in aged care.
Through our regulatory work, we monitor and assess compliance of aged care providers with their obligations to minimise the use of restrictive practices, including chemical restraint.
Providers must ensure that any restrictive practice is only used as a last resort, and in the least restrictive form, and for the shortest period of time to prevent harm to the resident. Additionally, a behaviour support plan must be in place for every consumer who is subject to a restrictive practice.
We have a range of resources available, including a psychotropic self-assessment tool and a Psychotropic medications use in Australia – information for aged care guide for providers, as well as resources on psychotropic medicines for consumers, their families and representatives which have been developed in partnership with the Older Persons Advocacy Network (OPAN).
Visit our Better use of medication on aged care webpage for more information.
Our latest ‘Sector performance report’ is now available
Our ‘Sector performance report’ for the October–December 2021 quarter is now available.
These quarterly reports include aged care sector performance statistics regarding residential aged care and home care services. They also report data related to the Commission’s regulatory and complaints functions, including complaints, applications to become an approved provider, accreditation, and assessed performance against the Aged Care Quality Standards.
To illustrate the utility of this publication for providers as an opportunity to analyse and compare a particular service’s performance, below is a summary of the data on complaints received about residential aged care services in the period October to December 2021.
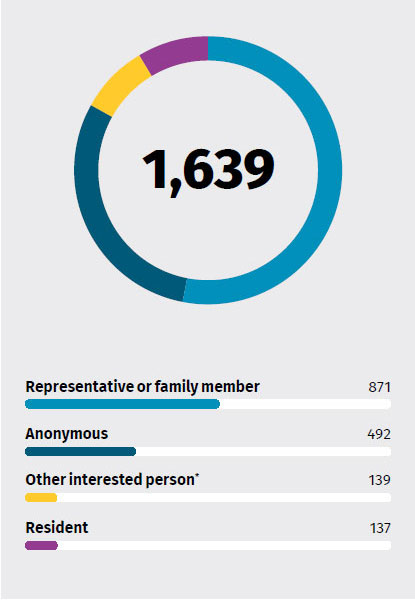
Complaints by complainant
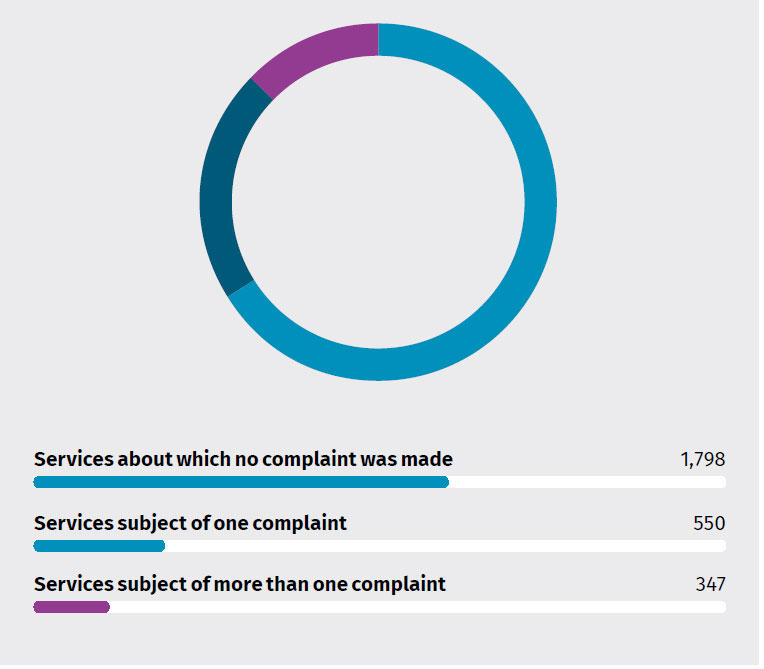
Residential services subject of complaints to the Commission
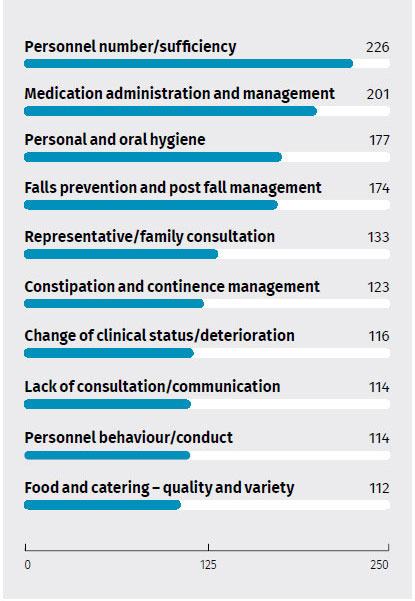
Top 10 complaint issues
Read our latest report for more sector performance information.
New and updated Commission resources
- New: Open disclosure consumer guide and A3 poster and open disclosure consumer video
- New: Appointing an advisor fact sheet
- New: Prudential Standards – Governance Standard fact sheet
- Updated: Regulatory Bulletin – Assessment contacts in residential and home services (RB2020-09) – The Commission uses a range of regulatory tools to monitor compliance with provider responsibilities and detect possible non-compliance. Assessment contacts are an example of a regulatory tool for these purposes. This updated Regulatory Bulletin outlines the Commission’s processes and responsibilities in relation to assessment contacts with accredited services (previously accredited services and home services). It now includes information regarding targeted assessment contacts, the management of infection risks and the publication of compliance information.